
Nutrition and Gout
What is Gout?
Gout is a common type of inflammatory arthritis.
When there are high levels of uric acid in the blood (hyperuricaemia), urate crystals can deposit and accumulate in joints causing a Gout attack. It's important to know that most people who have hyperuricaemia will not develop Gout.
So where do the high levels of uric acid in the blood come from?
The body produces uric acid when it breaks down purines - substances that are found naturally in your body and also in some foods that we eat.
Ordinarily, uric acid dissolves in the blood and passes through the kidneys and is removed in the urine. However, the body can sometimes be overwhelmed when:
- the body produces too much uric acid or
- the kidneys excrete too little
When uric acid to builds up in the blood, sharp, razorlike urate crystals can deposit in joints. This causes severe pain and inflammation (swelling, heat and redness) in the surrounding tissue. The joint becomes stiff and movement becomes difficult and painful. This is Gout.

Which joints does Gout affect?
Whilst gout can affect different joints, it usually occurs in only one joint at a time, most often the big toe. Other affected joints can include: other toes, the forefoot, ankles, knees, fingers, wrists, and elbows.
Signs and Symptoms
The symptoms of Gout can come and go. Typically, there are long periods of remission (no symptoms) lasting months to years, and flares (active inflammation) that can last for weeks. The onset of Gout symptoms happens suddenly, often in the big toe, and in the middle of the night. It is often described as feeling like the big toe is on fire.
Inflammation causes the affected joint to be swollen, hot, red and very tender, making walking (or using your hands) very difficult. As the gout attack progresses the pain gradually subsides to a feeling of lingering discomfort which can last for weeks.
Some people may only ever experience one episode of Gout, however, it is common for people to have repeated bouts.
It is important to seek medical treatment for any Gout flares.
If left untreated, over time they can lead to more frequent, longer lasting,
more painful episodes that permanently damage the joint, resulting in painful, limited
movement and reduced quality of life.

Risk Factors for Gout
Gout develops from high levels of uric acid in the blood. Factors that can increase the level of uric acid include:
Family history:
A family history of gout increases your risk of developing Gout.
Age and sex:
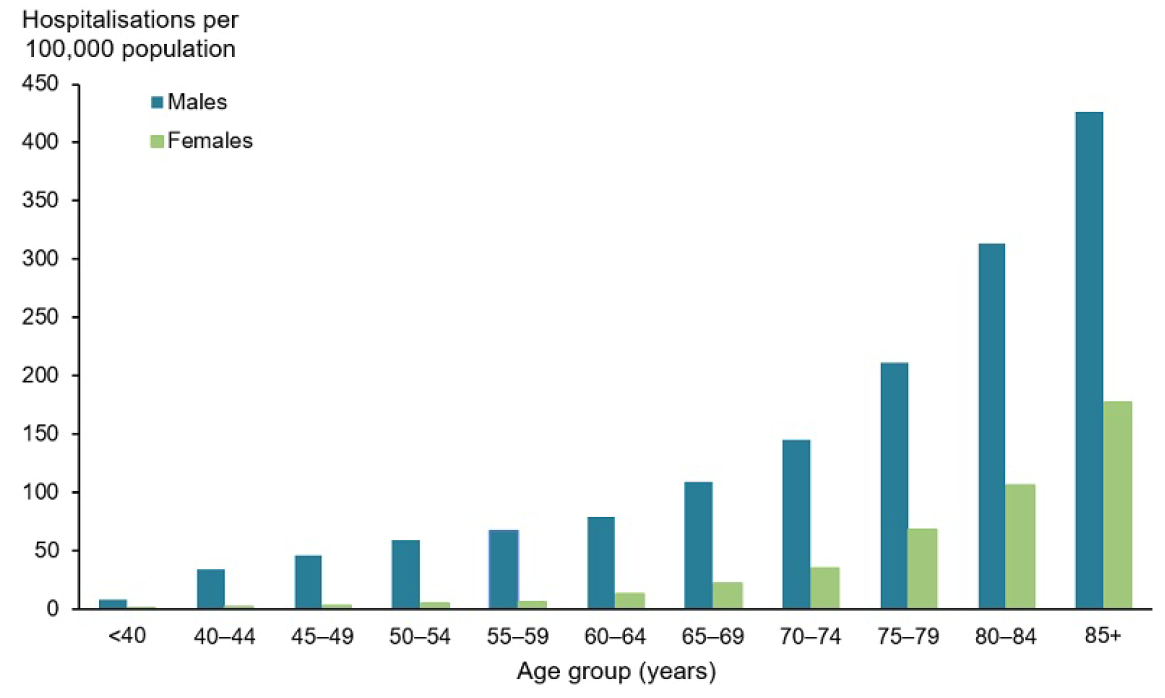
Whilst Gout can affect anyone, it is more common in males, 80% of cases are in men, and the risk increases with age.
Post-menopausal women make up the bulk of the other 20% of cases. Pre-menopausal women generally have lower
levels of uric acid, however, after menopause uric acid levels climb and are
similar to those of men. The graph below,
of hospitalisation of patients with Gout, is indicative of the typical
distribution of Gout within the Australian adult population.
Medical conditions
Some medical conditions, often co-morbidities of obesity, can increase your risk of gout. These include:
- high blood pressure
- insulin resistance and diabetes
- metabolic syndrome
- heart disease
- kidney disease - can reduce the body's ability to remove waste products including uric acid
Obesity and crash dieting
Gout was historically referred to as a 'King's Disease' as it is closely associated with the consumption of large amounts of fatty foods and alcohol, as well as obesity.
- Obesity - theories explaining this relationship include the metabolic activity of abdominal fat stores increases levels of inflammation in the body, as fat cells produce pro-inflammatory cytokines (chemical messengers)
- Crash dieting and rapid weight loss - leads to the accelerated breakdown of purine-containing body tissue and can significantly increase the levels of uric acid in the blood
Diet and lifestyle
Having a diet high in purine-rich food and drinking alcohol may increase the levels uric acid that contribute to Gout.

The Role of Nutrition
The dietary management of Gout has a couple of goals:
- to reduce the amount of uric acid in the blood
- to achieve and maintain a healthy weight
Traditionally, the primary dietary recommendation has been to follow a low-purine diet. However, completely removing purine-rich foods is unnecessary and may reduce the intake of important nutrients.
Moderating intake of the following purine-rich foods may be helpful:
- red meat - especially game meat
- offal / organ meat
- some seafood - including mackerel, anchovies, sardines, mussels, scallops, and tuna
- alcohol - particularly beer and spirits
- fructose sweetened drinks
- food and drinks sweetened with high fructose corn syrup (HFCS) - In Australia HFCS is not used extensively in convenience / processed food and soft drink manufacturing - however, limiting intake of these types of foods is always recommended for general health and weight management
Importantly, managing Gout isn't just about what foods to limit, but what foods we should be including. Research shows that the following purine-rich foods appear to be protective against Gout:
- purine-rich vegetables, which include mushrooms and spinach
- dairy foods
General recommendations for effective nutrition strategies for managing Gout include eating a diet high in:
- fruit
- vegetables
- plant proteins
- whole grains
- low-fat dairy products

It's no secret that here at Pulse Dietetics, we are big fans of the Mediterranean Diet. We are monitoring the latest research which includes the role of the Mediterranean and DASH* Diets in managing Gout, which so far looks very positive. We'll keep you posted.
*DASH = Dietary Approaches to Stop Hypertension
(high blood pressure)
Let's not forget water.
As uric acid is removed from the body in our urine, staying well
hydrated is especially important if you have Gout. So, drink plenty of water. However, if you are taking diuretics, have fluid
restrictions, or have impaired kidney function, consult with your doctor about
the amount of fluid that is best for you.

Long-term medical management of Gout
Whilst diet and lifestyle modifications are important to assist with the long-term management of Gout, they do not replace the medications prescribed by your GP or specialist.
If you are experiencing a gout flare you should seek medical treatment as soon as possible and follow the directions of your doctor. Your doctor may also prescribe medication for you to take to prevent future flares.

At Pulse, our mission is to cut through confusing and often conflicting nutrition information to give you the facts you need to help you manage your health.
Not only is our nutrition advice clear, straightforward and easy to understand, it is tailored to you and your lifestyle.
If you would like to find out how we can help
you manage Gout, we would love to hear from you. Just click on the link below
